78 year old male with abdominal pain and reduced urine output.
A 78/M WITH ABDOMINAL PAIN AND REDUCED URINE OUTPUT
No Icterus, cyanosis, clubbing, lymphoadenopathy
ICU bed 2
SOAP NOTES DAY 3
S
C/O abdominal pain decreased
O
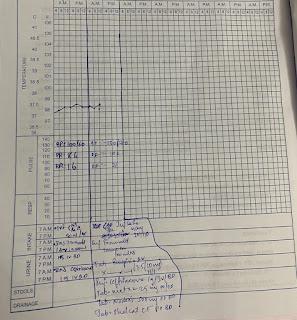
VITALS -
Temp - 98.5
PR - 96 BPM
BP - 100/80 MM OF HG
RR - 22
SPO2 - 100% @5 lits O2
GE
Patient is conscious coherent cooperative well oriented to time place and person
Pallor +
No Icterus, cyanosis, clubbing, lymphoadenopathy
SYSTEMIC EXAMINATION -
PA : DISTENDED, umblicus inverted SOFT, tenderness decreased in Rt lumbar, Right hypochondrium
CVS : S1 AND S2 HEARD , NO MURMURS
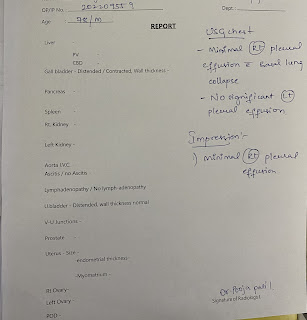
RS : BILATERAL AIR ENTRY PRESENT, decreased breath sounds - Rt IAA, IMA
CNS : NAD
HEMOGRAM
HB 10.7
TC 12,600
PLT 1.60
MCV 85
SMEAR - NORMOCYTIC NORMOCHROMIC Anemia with neutrophilic leucocytosis
RFT
Urea 90
Creatinine 2.6
A
HFrEF (EF-34%)
Peripheral vascular disease with cor pulmonale with k/c/o CAD s/p PTCA(10years back) with CKD on conservative management with left sided hearing loss (on hearing aid since 6 years) ?congestive hepatopathy.
P:-
Inj. Lasix 40mg IV SOS if SBP >130MMHG
T. Ecosprin AV 75/10 mg PO HS
T. Met-XL 25 MG PO OD
T. Nodosis 500 mg PO BD
T. Orofer XT PO OD
T. Shelcal 500 mg PO OD
Intermittent CPAP
Inj. Ceftriaxone 1g IV BD (day 3)
|
|
Day1 |
Day2 |
Day3 |
|
TLC |
17,100 |
6,400 |
12,600 |
|
Sr. UREA |
47 |
78 |
90 |
|
Sr. Creatinine |
2.2 |
2.5 |
2.6 |
ICU bed 2
SOAP NOTES DAY 4
S
C/O abdominal pain decreased
O
VITALS -
Temp - 98.5
PR - 96 BPM
BP - 110/80 MM OF HG
RR - 22
SPO2 - 100% @5 lits O2
GE
Patient is conscious coherent cooperative well oriented to time place and person
Pallor +
No Icterus, cyanosis, clubbing, lymphoadenopathy
SYSTEMIC EXAMINATION -
PA : DISTENDED, umblicus inverted SOFT, tenderness decreased in Rt lumbar, Right hypochondrium
CVS : S1 AND S2 HEARD , NO MURMURS
RS : BILATERAL AIR ENTRY PRESENT, decreased breath sounds - Rt IAA, IMA
CNS : NAD
HEMOGRAM
HB 11.5
TC 16,400
PLT 1.50
MCV 85
SMEAR - NORMOCYTIC NORMOCHROMIC Anemia
RFT
Urea 91
Creatinine 2.5
ECG at 9am- ventricular trigeminy
|
|
Day1 |
Day2 |
Day3 |
Day4 |
|
TLC |
17,100 |
6,400 |
12,600 |
16,400 |
|
Sr. UREA |
47 |
78 |
90 |
91 |
|
Sr. Creatinine |
2.2 |
2.5 |
2.6 |
2.5 |
A
HFrEF (EF-34%)
Peripheral vascular disease with cor pulmonale with k/c/o CAD s/p PTCA(10years back) with CKD on conservative management with left sided hearing loss (on hearing aid since 6 years) with Acute acalculus cholecystitis
P:-
Inj. Lasix 40mg IV SOS if SBP >130MMHG
T. Ecosprin AV 75/10 mg PO HS
T. Met-XL 25 MG PO OD
T. Nodosis 500 mg PO BD
T. Orofer XT PO OD
T. Shelcal 500 mg PO OD
Intermittent CPAP
Inj. Ceftriaxone 1g IV BD (day 4)
https://sravanivv180.blogspot.com/2022/03/78-year-old-male-with-abdominal-pain.html
ICU bed 2
SOAP NOTES DAY 5
S
C/O abdominal pain and tenderness present in right hypochondrium
O
VITALS -
Temp - 98.1
PR - 79 BPM
BP - 110/70 MM OF HG
RR - 22
SPO2 - 100% @5 lits O2
GE
Patient is conscious coherent cooperative well oriented to time place and person
Pallor +
No Icterus, cyanosis, clubbing, lymphoadenopathy
SYSTEMIC EXAMINATION -
PA : DISTENDED, umblicus inverted SOFT, tenderness present in Rt lumbar, Right hypochondrium, Bowel sounds present. Stools passed . No fever spikes
CVS : S1 AND S2 HEARD , NO MURMURS
RS : BILATERAL AIR ENTRY PRESENT, decreased breath sounds - Rt IAA, IMA
CNS : NAD
HEMOGRAM
HB 11.5
TC 14,600
PLT 1.54
MCV 83.8
SMEAR - NORMOCYTIC NORMOCHROMIC Anemia with leukocytosis.
RFT
Urea 90
Creatinine 2.2
Day1 | Day2 | Day3 | Day4 | Day 5 | |
TLC | 17,100 | 6,400 | 12,600 | 16,400 | 14,600 |
Sr. UREA | 47 | 78 | 90 | 91 | 90 |
Sr. Creatinine | 2.2 | 2.5 | 2.6 | 2.5 | 2.2 |
A
HFrEF (EF-34%)
Peripheral vascular disease with cor pulmonale with k/c/o CAD s/p PTCA(10years back) with CKD on conservative management with left sided hearing loss (on hearing aid since 6 years) with acute acalculus cholecystitis.
P:-
Propped up position
Fluid and salt restriction
Inj. Lasix 40mg IV TID 8am--2pm--8pm
T. Ecosprin AV 75/10 mg PO HS
T. Met-XL 25 MG PO BD
T. Nodosis 500 mg PO SOS
T. Livogen 1 tab PO OD
T. Shelcal 500 mg PO BD
Inj. Tramadol 1 amp in 100 ml NS IV TID
Intermittent CPAP
Inj. Ceftriaxone 1g IV BD(Day 5)
Inj. Thiamine 1amp in 50 ml NS IV OD














Comments
Post a Comment